The use of mice as ‘models’ for testing drugs intended for use in humans is ‘nearly useless’, according to an article in the prestigious science journal Nature.
In the past year alone, three major potential new drugs for Alzheimer’s disease that appeared very promising in mouse ‘models’ of the disease failed in clinical trials. Although scientists can create mice with deformities resembling those seen in patients’ brains, the mice do not have dementia, and drugs that target these deformities have repeatedly failed in human trials, causing scientists to question whether the mice truly mimic what happens in the human brain.
Worse, almost a dozen drugs that helped mice with amyotrophic lateral sclerosis (ALS), a progressive, usually fatal disease of the nerves, to live longer have failed or even harmed humans:
‘In the most recent and spectacular of these failures, [a drug] which had seemed modestly effective in four separate ALS mouse studies since 2002, was found last year to have worsened symptoms in a clinical trial of more than 400 patients.’
There are no good mouse models for Parkinson’s disease, and even the mouse model for Huntington’s disease, which has a simple genetic cause, does not suffer from all the same symptoms. This shows yet again how recreating even a seemingly straightforward genetic fault in another species cannot be relied upon to mimic the human condition, because the background biology of each species is just too different and complex.
According to neurologist Dr Michael Benatar, from Emory University School of Medicine in the US:
‘I think there’s a sense of desperation that we need a convenient model for bringing drugs to clinical trial. But desperation is an inadequate justification for the continued use of a poor model.
It’s a bit like the proverbial drunk who keeps looking for his lost keys under the lamp post, simply because the light’s better there.’
Reference: Nature 454: 682
An article in the prestigious science journal Nature discussed the now discredited use of anti-arrhythmia drugs after heart attacks. These drugs were supposed to save lives by reducing irregular heart beats.
Subsequent reviews of the outcomes for patients who had received these drugs, compared with those who had not, caused consternation when it was discovered that the drugs more than doubled the risk of death or heart attack:
‘Everyone was so confident that if you quieted the extra heartbeats, the patients would do better, but people died.’ Dr Harlan Krumholtz, Yale University.
‘It is not easy to think of a greater medical error, since the practice of therapeutic bleeding, than the use of antiarrhythmic drugs in patients after myocardial infarction.’ Robert Temple, director of the Office of Medical Policy at the US Food and Drug Administration (Clinical Measurement in Drug Evaluation, 1995).
The author reminded readers that the use of the drugs:
‘depends principally on tradition, on an unproven expectation that antiarrhythmic effects are likely to be beneficial for potentially lethal arrhythmias as well as for less malignant conditions, and on extrapolation from animal experiments.’ (Chamberlain, Heart 1998; 80: 408).
Reference: Nature 452, April 2008: 510.
 Adverse drug reactions cost NHS £2bn
Adverse drug reactions cost NHS £2bnCompass, a London-based thinktank, has revised the latest estimates for the cost of adverse drug reactions dramatically upwards.
According to Health Minister Dawn Primarolo, 6.5% of hospital admissions (well over a million) are as a result of bad reactions to prescription drugs. When the cost of caring for patients who become ill whilst already in hospital as a result of drugs they are prescribed is factored in, Compass estimates that the cost to the NHS is £2billion.
With the NHS coming under ever increasing pressure to provide expensive drugs to patients, it is imperative that the burden of adverse drug reactions be reduced. Part of the solution would be to introduce more personalised medicine (making use of genetic and other testing techniques to check whether a drug is suitable for a patient). Also, to ensure that only drugs with the best safety profiles are marketed, more extensive clinical trials need to be carried out, preceded by the most human-relevant laboratory tests.
Reference: the Guardian, 3rd April 2008.
Researchers writing in the journal Science have found, using test tube-based experiments, that unexpected uses for drugs may be identified by comparing the side effects they cause with those of other, unrelated drugs. This finding makes it even more important that accurate information about the side effects patients experience is collected and analysed.
Reference: Science, 321: 263, July 2008
 Mice are not men
Mice are not menA study published in the prestigious journal, the Proceedings of the National Academy of Sciences, in May has found that although humans and mice share about 85% of their genes, 22% of genes known to be essential in humans are not at all essential in mice. This casts serious doubt over the relevance of using mice to find out the roles of genes in humans.
Another study published in the Proceedings of the National Academy of Sciences (PNAS) in July showed that a gene which promotes colon cancer growth in mice has the opposite effect in human colon cancer cells. So a drug designed to suppress this gene or its protein product – based on its function in mice – might actually speed the growth of colon cancers in people.
References: PNAS 105:6987 and 105:9697
 Virtual children
Virtual children‘We now have a tool which allows complex clinical scenarios to be explored in the safety of a computer.’ Professor Amin Rostami
Testing medicines in children has always been difficult as they cannot give consent to participate in trials and parents are, naturally, wary of exposing their children to unknown risks. However, thanks to a computer model developed by Sheffield-based company Simcyp, it should now be much easier to calculate safe doses. This development could not have come at a better time after a new EU regulation demanding that medicines destined for children must now have been tested especially for them. This makes sense as it is now acknowledged that children cannot simply be treated as scaled-down adults:
‘In particular, children under two years old are the most physiologically different to adults, so it can be too simplistic to scale back from adult values when determining appropriate doses for children, as currently happens.’ Amin Rostami, Professor of Systems Pharmacology at the University of Sheffield and director of research and development at Simcyp.
Reference: The Times, July 28 2008.
 Animal pain research criticized
Animal pain research criticized‘In my research, animal models don’t represent human patients sufficiently well, and that’s a problem that extends across pain research as a whole. New and highly sophisticated brain-imaging technology is providing vital insights that animal research has failed to produce. I would like to see far greater uptake of these and other human-relevant approaches to pain research to help us develop the effective treatments that patients so desperately need.‘
Professor Qasim Aziz, Barts and the London School of Medicine and Dentistry.
A report in the journal Neuroimage has criticised the use of animals in pain research.
The report’s authors encouraged scientists to make better use of the latest technologies, such as MRI scanning, in ethically conducted studies in people who actually suffer from the pain they are trying to treat. The role of human tissues grown in the lab was also emphasised.
Pain research experts from leading institutes across the UK made these recommendations at a workshop organised by Focus on Alternatives, a coalition of notfor- profit organisations promoting non-animal research, including the UK Human Tissue bank and chaired by the Dr Hadwen Trust.
Reference: NeuroImage 42:467.
A review of the contribution of animal-based studies has failed to find significant agreement between the results seen in animals and in humans. The author examined an extensive list of published research, including experiments conducted on chimpanzees, and found that they were generally very poor at predicting human outcomes and contributed little to the development of successful human treatments.
Reference: Knight, Reviews on Recent Clinical Trials, 2008; 3(2): 89.
Scientists have reviewed the ability of animal tests to predict which drugs will harm patients’ livers and found that they miss dangerous chemicals around half of the time.
Perhaps surprisingly, non-rodents (such as pigs or monkeys) predicted human toxicity in many cases only 19% of the time, which is even less often than rodents (such as mice or rats), which can correlate as poorly as 46% of the time! These astonishing figures go some way towards explaining why 92% of drugs fail in human trials, despite undergoing extensive animal tests.
The pharmaceutical researchers who wrote the report, Species Concordance for Liver Injury, are part of an initiative known as the Safety Intelligence Program. They are currently trying to understand why the animal tests translated so poorly to humans; hopefully they will now look at human biology-based methods for predicting liver toxicity as a means of improving this abysmal track record.
Reference: Nature Reviews Drug Discovery 7:719, September 2008.
 Brain donors worth their weight in gold
Brain donors worth their weight in goldThe Parkinson’s Disease Society Tissue Bank, at Imperial College London opened five years ago to provide a vital resource to any researcher wishing to study Parkinson’s Disease. The bank has since received more than 250 brains. However, perhaps unsurprisingly, the majority of donors have been patients with Parkinson’s Disease, leaving a shortfall of only 17 ’control’ brains, which can be used for comparisons between the brains of sufferers and non-sufferers of this debilitating disease.
“Alzheimer’s, Parkinson’s and other neurodegenerative diseases occur in humans and it is in human tissue that we will find the answers to these diseases.” Dr. John Xuereb, Director, Cambridge Brain Bank Laboratory (BBC Radio Cambridgeshire, 2002).
For more information on becoming a donor, contact the UK Parkinson’s Disease Society Tissue Bank: 0207 594 9732, pdbank@imperial.ac.uk or visit www.parkinsons.org.uk
Read the whole article from the Times, 30th August 2008
VaxDesign Corporation
There is an urgent need for technologies that can mimic the human immune system, as time and again animal tests have shown that they are simply not up to the job. An excellent article in Time magazine on 27th March, showed how the answer has now arrived in the shape of a human-relevant, fast test that can be performed entirely by robots, developed by a Florida company called VaxDesign (www.vaxdesign.com).
According to William Warren, president, CEO and co-founder of VaxDesign:
“We know animal models do not translate to human responses…Animal models of treatments for HIV to psoriasis and flu are not representative of human responses” (TechJournal South, 2nd October 2007).
The scientists at VaxDesign saw this urgent need for something that was more relevant to people and the MIMIC (Modular IMmune In vitro Constructs) system was born.
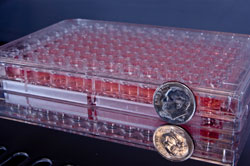
MIMIC uses plastic dishes with almost 100 wells in which cells from different human blood samples are grown. This means that you can effectively test the impact of a new vaccine on hundreds of humans, safely and rapidly, before a single volunteer has to be exposed! Scientists at the company are confident that this revolutionary technology therefore offers benefits that animal tests can never hope to provide. Michael Rivard, vice president of corporate development at VaxDesign says that:
“The information you get from this type of test is far and beyond what you’d get out of a mouse study, both because it’s humans and because you can see the effect across a spectrum of genotypes (different genetic make-ups).” (quoted in Time magazine, 27th March)
In March, the International AIDS Vaccine Initiative bestowed its first ever Innovation Award on VaxDesign. Their approach is supported by Wayne Koff, senior vice president of research and development at the International AIDS Vaccine Initiative, who commented:
“In the end, you can only extrapolate so much from a monkey model.” (quoted in Time magazine, 27th March)
Meanwhile, many AIDS vaccine researchers (and their funders) appear determined to keep their heads buried in the sand. In the wake of several high profile vaccine failures, some of which actually increased the risk of infection with HIV, doubts about our ability to produce a vaccine have resurfaced:
“Despite hundreds and hundreds of millions of dollars, the reality in 2008 is that an HIV vaccine clearly remains beyond our grasp.” Prof Warner C. Greene, University of California, San Francisco (quoted in The Baltimore Sun, 26th March).
This has led to calls on some sides to focus resources on proven strategies to help prevent the spread of infection and provide drugs to those who need them.
“I think we should pull the plug on vaccine research. Do we have any other enterprise that has been studied for 25 years and for which we’ve spent billions of dollars where we have no results?” Michael Weinstein, President of the AIDS Healthcare Foundation (quoted in The Washington Post, 26th March).
Clearly the focus needs to be on patients and human biology-based research, rather than on attempting to improve animal “models” and tests.
“When it comes to testing HIV vaccines, only humans will do.” Alison Tonks, British Medical Journal, 2007;334;1346.
A poll conducted by the Independent has revealed that most leading AIDS researchers are deeply pessimistic about the prospects for developing a truly effective vaccine within 10 – 20 years (if ever). Moreover, Anthony Fauci, director of the US National Institute of Allergy and Infectious Diseases (NIAID) told the Independent that:
“We’ve learnt a few important things [from the clinical trial]. We’ve learnt that one of the animal models, the SHIV [an artificial virus meant to mimic the human virus but capable of infecting monkeys] model, really doesn’t predict very well at all. At least we now know that you can get a situation where it looks like you are protecting against SHIV and you’re not protecting at all in the human model – that’s important.” (the Independent, 24th April)
Yet despite accepting that the major animal model for AIDS is not predictive for humans, and significant doubts about the ability of tests in animals to ever produce a successful vaccine, the US NIAID has vowed to continue to fund and promote much more basic research… in animals.
“We will not discontinue research, period. Not only will we not decrease it, we will in fact try to increase it.” Dr. Anthony S. Fauci, director of the NIAID (quoted in The Baltimore Sun, 26th March).
This is particularly alarming given that about a third of the NIAID’s £1.45 billion budget goes on HIV vaccine research. Let’s hope that the other agencies rethink their strategy along the lines of the International AIDS Vaccine Initiative, which is supporting VaxDesign’s human immune system in a test-tube, and whose senior vice president of research and development asserted:
“[getting from small animal studies to monkeys] takes a lot of time, and, with HIV, we don’t have a lot of time. We asked the question is there a way to do it faster and take it to humans more quickly?” (quoted in Time magazine, 27th March)
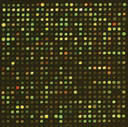
Following the revolutionary US National Research Council report published last June (http://safermedicines.org/reports/toxicitytesting.shtml), three agencies — the Environmental Protection Agency, the National Toxicology Program and the National Institutes of Health — have outlined a collaboration to replace animal tests with faster, cheaper and more human-relevant methods, using many of the technologies that are already available (published in top journal Science, 15th February 2008).
Almost 3,000 environmental chemicals are now being screened in over 50 cell-based tests. The results will then be compared with information already gleaned from humans and past animal tests. A highly encouraging study has already put over 1,400 chemicals through a battery of 13 cell-based tests. Unsurprisingly, they found differences between the way in which human and animal cells reacted: ‘A striking finding from the current study is the lack of similarity in the patterns of compound activity in cells derived from the same tissue but from different species’ (NIH scientists Menghang Xia & colleagues, Environmental Health Perspectives, March 2008). Surely this illustrates how important it is to focus on using human cells as it is humans that must be mimicked.
Discussing this ground-breaking venture, Dr. Francis Collins, who led the publicly funded project to sequence the human genome and is now the Director of the National Human Genome Research Institute, told reporters at an American Association for the Advancement of Science conference: ‘We are not rats and we are not even other primates… After all, ultimately what you are looking for is, does this compound do damage to cells? Can we, instead of looking at a whole animal, look at cells from different organs?’
He was backed up by another eminent scientist, Dr Christopher Austin, Director of the National Institutes of Health Chemical Genomics Center, who explained that ‘Traditional animal testing is expensive, time-consuming, uses a lot of animals and from a scientific perspective the results do not necessarily translate to humans.’
 Rodent test proven redundant
Rodent test proven redundantScientists from 18 pharmaceutical companies and the UK NC3Rs (National Centre for the Replacement, Refinement and Reduction of Animals in Research) have collaborated to publish a review of acute toxicity tests in animals in the journal Regulatory Toxicology and Pharmacology. The study shows that the single dose acute toxicity test – long campaigned against by anti-vivisectionists – is in fact redundant.
The test is supposed to determine whether a drug is too toxic to proceed with, which organs it affects and what starting dose to use in clinical trials. However, the study found that it fulfils none of these objectives. The authors hope that their evidence will persuade regulatory agencies that the test should no longer be required.
This groundbreaking study highlights the need to evaluate the supposed value of other animal tests that are still used before new drugs enter humans.
 Root cause of childhood leukaemia discovered
Root cause of childhood leukaemia discoveredResearchers have identified a key cell in the bone marrow which, when combined with a second mutation, leads to childhood leukaemia. Scientists were only able to make this breakthrough by studying 4 year old twin girls, one of whom has developed leukaemia while the other (thus far) remains free of the disease.
Dr Bruce Morland, consultant paediatric oncologist at Birmingham Children’s Hospital and chairman of the Children’s Cancer and Leukaemia Group, said:
‘The identification of the leukaemic stem cell has been one of the ‘Holy Grails’ for cancer biologists and this study certainly brings us one step closer.’
Professor Vaskar Saha, professor of paediatric oncology at Cancer Research UK commented:
‘This important paper shows how leukaemia develops, and how it can persist even after therapy. By identifying the cells involved, it raises the hope that we will be able to identify children at risk of relapse, and develop new, targeted drugs to treat the disease.’
 CEO of Eli Lilly calls for drug safety revolution
CEO of Eli Lilly calls for drug safety revolutionSpeaking in October in the US, the head of pharmaceutical company Eli Lilly, Sidney Taurel, called for major improvements in the way in which post-marketing drug surveillance is carried out.
‘The use of prescription medicines always will be a matter of balancing benefits and risks. Fortunately, systems are now within our grasp to more quickly identify both the true benefits and the full extent of risks associated with medicines in widespread use.’
Sidney Taurel accused the US FDA, medical professionals and industry of failing to collaborate and take advantage of the latest information technologies in order to ensure that drugs are adequately followed once they have been released onto the market.
Phase IV (post-marketing) clinical trials are lengthy and expensive but extremely important as very rare side effects may only be detected once a drug has been taken by many thousands of patients. Approximately half of all drugs that make it to market are withdrawn or relabelled due to unforeseen side effects, and it is vital that these side effects are picked up as swiftly as possible.
Currently, more than 1,200 commitments (89% of those made) by companies to conduct post-marketing safety assessments remain unfulfilled in the US alone. Usually the system relies on doctors reporting instances where they suspect their patients have suffered an adverse reaction to a treatment; in the UK this is known as the Yellow Card system. However, it has long been acknowledged that as few as 1-10% of adverse drug reactions are reported.
A failure by doctors to make the difficult distinction between adverse reactions and disease symptoms can prove potentially fatal, as patients may be given drugs that are more harmful than helpful. The incidence of deaths from prescription drugs has more than doubled in 10 years, according to figures published in October. Dr Peter Maguire, deputy chairman of the BMA Board of Science, said:
‘This big rise in fatal and serious adverse drug reactions should be a wake-up call to all doctors.’
In the 10 years to 2005 the number of prescriptions rose from 485m to 752m, and the cost to the NHS from £4bn to £8.2bn. Labour MP Paul Flynn warned:
‘We are heading towards pharmageddon’ (the prospect of a world in which medicine produces more ill health than health).
 Diabetes drug causes heart failure
Diabetes drug causes heart failureWith disturbing echoes of the Vioxx debacle, another blockbuster drug, Avandia, has been found to increase the risk of congestive heart failure and heart attack – by as much as 72% in patients with a history of heart disease.
Dr. David Graham, associate director for science and medicine at the FDA, testified that:
‘…In the nearly eight years that Avandia has been sold, it has caused roughly 80,000 additional sudden cardiac deaths and nonfatal heart attacks.’
Disturbingly, it seems that Avandia’s manufacturer, GlaxoSmithKline, has been aware of an increase in cardiac risk since 2000 and, along with the FDA, threatened scientists who tried to raise the alarm about the drug. US Congressman Bart Stupak observed:
‘the FDA’s apparently callous disregard for the safety of diabetics taking Avandia is very reminiscent of the Agency’s failure to move on Vioxx when substantial safety signals first became known.’
Avandia has also been found to increase the risk of a serious eye condition, macular oedema, and bone fractures in women.
It is clear that insufficient testing of the drug’s effects in humans took place both before and after marketing. Dr Ike Iheanacho, editor of the Drug and Therapeutics Bulletin commented wryly:
‘Having produced a new treatment, drug companies take great care to avoid testing it too exhaustively in patients …Sometimes, for the drug industry, ignorance is bliss.’
The DataChip is a new biochip containing more than 1,000 human 3D cell cultures arranged to mimic the human body. Scientists at the University of California collaborated with Solidus Bioscience in the US to design a rapid, cheap, automatable way of screening new drugs in a much more complex and realistic way than that provided by individual 2D cell cultures. The Datachip incorporates liver tissue cultures as the liver has an important role in breaking down drugs, sometimes altering their toxicity or potency. One of the exciting things about the DataChip is that it could be modified to reflect the make-up of individual patients, leading to more personalised medicine.
 Virtual TB cell
Virtual TB cellPresently, no one really understands why most of the bacteria which cause tuberculosis succumb to drugs within weeks whilst a stubborn population can continue to cling on for months. In an effort to understand this better, scientists at the University of Surrey have created a virtual bacterium on computer, which they hope will greatly speed up the search for new drugs. The model has been validated by testing real-world scenarios which show that the model responds in the same way in which the bacterium is known to behave.
 More scanner news
More scanner news‘It is so powerful it can capture an image of the entire heart in just two beats’ – Steve Rusckowski, chief executive of Philips Medical Systems
In November a new CT (Computed Tomography) scanner that uses only a fraction of the X-ray radiation normally required to produce a CT image of the body was unveiled by Philips in the US. The Brilliance CT generates a 3D rotatable image of the body more quickly than an ordinary CT scan and in much greater detail. This could be very useful when looking to see if cancers have spread, for example.
 Cancer tissue bank opens
Cancer tissue bank opens‘Samples of tissue and body fluids from patients are fast becoming the cornerstone of cancer research’ – Professor Herbie Newell, Cancer Research UK
OnCore UK is a national resource that aims to collect samples of every type of cancer from all tissues of the body for research. Patients at a limited number of NHS Trusts can now donate removed tissue, and the scheme should soon be rolled out across the UK, enabling patients to directly contribute to the search for treatments if they wish. The bank will also liaise with other existing tissue banks. Cancers come in many forms, so the more samples researchers have at their disposal the more relevant information can be gleaned and the more confidence scientists can have that their results will apply to patients.
 AIDS vaccine woes continue
AIDS vaccine woes continue‘Mice lie, monkeys sometimes lie, and humans never lie. Some monkeys have lied to us this time’ Peggy Johnston, head of the US National Institutes of Health’s AIDS vaccine programme
20 years after the first successful AIDS drug, AZT, was discovered by testing cells in petri dishes, the struggle to find a successful vaccine against the virus that causes AIDS continues to fail. In October a new vaccine made by Merck which uses a virus related to the common cold as a delivery system was withdrawn from trials after it was found to actually increase the rate of infection.
More promising is the news that Harvard scientists have identified 273 potential new HIV targets (for drugs) by studying thousands of human genes in test tubes.
Likewise, the introduction of a genetic test for an anti-HIV drug, Ziagen (also known as Abacavir), means that patients will now be able to take the drug safely – or if they are unsuited, they can find this out before risking their lives and take a different drug instead. This test is necessary because a clinical trial showed that patients with a certain genetic mutation develop a potentially life-threatening heart problem.
 Hepatitis C virus begins to yield secrets
Hepatitis C virus begins to yield secretsHepatitis C is a virus that can be spread through bodily fluids such as blood. According to the British Liver Trust, 20% of patients with a chronic infection go on to need a liver transplant due to severe liver damage and consequently liver cancer or liver failure.
Scientists at the University of Birmingham studying human liver tumour cells infected in the lab with the Hepatitis C virus have discovered that the virus can spread directly from cell to cell, a discovery which sheds light on its ability to evade the immune system. This had never been observed before in Hepatitis C and will inform future research efforts to target the virus.
 Stem cells for safer medicines
Stem cells for safer medicinesStem Cells for Safer Medicines (SC4SM), a not-for-profit company, was founded in October by the Department of Health and the Association of the British Pharmaceutical Industry (ABPI). Human stem cell technology will allow for much more predictability in terms of screening out compounds that will be toxic to the liver, said a spokesperson for the ABPI, adding that ‘currently it’s not much better than tossing a coin’.
Capsant Neurotechnologies Ltd, with Southampton University and King’s College, London are using 3D human stem cells to test new drugs. Professor Lars Sundstrom, Chief Scientific Officer of Capsant, commented:
‘Essentially, we are making mini-organs in a dish so that the testing of new pharmaceutical products can be carried out more accurately.’
In December scientists in the US revealed a human embryonic stem cell test for predicting drug effects on the foetus. They found a specific cell response to drugs that have been linked to autism when prescribed to pregnant women.
 Alzheimer’s Disease mice fail to mimic humanresponses to drugs
Alzheimer’s Disease mice fail to mimic humanresponses to drugs‘Testing drugs against AD on animals is not easy because animals don’t develop the disease’ – Professor Sascha Weggen, Heinrich-Heine-University, Germany
In August, scientists in America studying breeds of mouse supposed to mimic Alzheimer’s Disease reported that some fail to respond to treatments already used in patients (Journal of Biological Chemistry). The researchers admitted that this mismatch between outcomes in mice and humans could lead to effective drugs being missed, stating that: ‘These compounds may seem to be ineffective on these mice, while it’s actually the mouse breed that is to blame.’
Furthermore, the researchers acknowledged that studying drugs in such mice simply won’t provide insight into what happens in patients’ brains:
‘Our study shows that these mouse breeds may not reflect what may really happen in the brains of Alzheimer’s patients if they were treated with such compounds in future clinical studies.’
This study echoes findings by US National Cancer Institute scientists in 1997 that xenograft mice models, where human tumours are grown in immunecompromised mice, miss effective cancer treatments.
 Gene regulation differs hugely between the mouse and human liver
Gene regulation differs hugely between the mouse and human liverMice and humans may share over 90% of their genes, but vital differences exist in how those genes are turned on or off. Scientists at the Massachusetts Institute of Technology have now quantified these differences for the liver, and found variations in up to 89% of the sites they examined.
By harnessing the latest DNA technology researchers have developed a better way to study the parasites that cause bilharzia, a serious disease affecting the developing world. Instead of infecting rodents with the parasites, the new method involves collecting samples directly from infected people. The work has been awarded the NC3Rs 3Rs Prize 2007.
This will clearly lead to a better understanding of the disease, which should help to combat it more effectively. Study leader, Dr Charlotte Gower, said:
‘Using the non-animal techniques has also improved our scientific results because we can now reflect the genetic variation in the natural population of parasites. We demonstrated that the traditional method of growing parasites can bias results by skewing the genetic variation.’
 Major progress through large genetic studies
Major progress through large genetic studiesEpidemiology – the study of populations has long been used to reveal the links between diseases and environmental or dietary risk factors, for example between smoking and lung cancer, low levels of folic acid during pregnancy and spina bifida, asbestos and cancer, etc. Now population studies are being linked with genetic analyses to find out which gene forms predispose people to certain diseases.
In 2007, researchers began to discover the extent to which our genomes differ from person to person and the implications of this variation for deciphering the genetics of complex diseases. Techniques that scan for hundreds of thousands of genetic differences at once are linking particular variations to particular diseases in ways that were simply not possible before.
In a hugely significant study, Wellcome Trust scientists analysed blood samples from over 17,000 people in an effort to link genes with common diseases, and their efforts have paid off handsomely. In June, they reported finding genes linked with depression, Crohn’s disease, coronary heart disease, hypertension, rheumatoid arthritis and both type 1 and 2 diabetes. This research could lead to tests to identify those most at risk of developing these diseases, and may eventually lead the way to targets for new drugs.
Recent months have brought exciting news in the endeavour to link genetics and bowel cancer: using whole genome analyses, researchers in London and Edinburgh identified a gene form that increases the risk of developing bowel cancer by 20% (July 2007), while at the end of 2007, Cancer Research UK scientists discovered two new mutations that seem to triple the risk of developing bowel cancer. These discoveries may eventually be incorporated into a screening programme to identify those most at risk in order to ensure they are monitored appropriately.
An international team of researchers identified a gene variant that appears to predispose children to asthma. This was accomplished by comparing DNA from over 900 asthmatics with more than 1,200 healthy volunteers (July 2007).
September 2007 was a good month in the effort to link genes and cancers:
Italian and UK scientists studying breast cancer biopsies have identified a gene that is turned on at lower levels in particularly aggressive breast cancers. In the future it may be possible to test patients for the activity of this gene in order to decide which women need the most intensive treatment, thus minimising side effects to women who do not need the most aggressive treatments and ensuring that those who do need it receive it sooner.
A genetic test for prostate cancer was announced by Gen-Probe. The current test which looks for a protein called Prostate Specific Antigen in the blood has a high false-positive rate, without picking up all actual cancers, meaning that men may have to have extra tests, with all the unnecessary extra stress that an uncertain diagnosis causes. This new test measures the activity of a gene which is only turned up in prostate cancer. Unfortunately, at this stage it will probably only be made available to men thought to be at high risk of the disease because of the cost (£200 versus £10 for the conventional test).
Scientists in Aberdeen announced that they have identified two genes that can be used to predict when a patient’s breast cancer will not respond to a treatment – docetaxel. The researchers made their discovery by studying samples of tumours from patients in the lab, and are now looking to see whether their results will apply to new patients. This discovery brings personalised medicine a step closer, and could reduce the time taken to identify which drug will work for a patient, increasing the likelihood of success and eliminating the need to suffer side effects from drugs that will not help anyway. UK researchers are currently embarking on a massive study, including 14,000 volunteers, to find out which genes are associated with osteoarthritis, which affects more than 2 million people in the UK alone. Currently, there are no drugs to treat this painful, debilitating disease, so patients must rely on painkillers – which are not without risk (eg. Vioxx). If genetic factors can be uncovered this will inspire the search for effective new drugs.